Exercises for Plantar Fasciitis

… more than simple foot stretches!
Plantar fasciitis is one of the most persistent and common running overuse injuries that can occur anywhere from youth to our latter decades. A 2008 study estimated that about 10% of the general population will experience plantar fasciitis at some point in their lifetime. From a quick perusing of the internet, the commonly encountered advice for plantar fasciitis is focused around stretching, tennis ball and ice massage, and night braces for Plantar Fasciitis.
I’m about to give you a few “physical therapist pearls” on plantar fasciitis that may surprise you.
- Don’t believe everything you find on google. Many of the internet “research” out there is inaccurate and outdated. I’m going to provide you with the latest evidence in this article.
- Expect to put in the time and effort if you want to find a treatment that provides lasting relief. Our culture often seeks a “quick fix” when it comes to injuries, especially when they are preventing us from functioning in daily activities or from doing what we love. Be very wary of medical professionals who recommend surgical approaches, injections or medications without an ACTIVE approach first. That translates to putting the time in for exercises and getting at the root cause of the issue, not just putting a “band-aid” on it. And, expect the treatment to take time. Most studies analyze patient outcomes after a minimum of 3 months of treatment. Recovery is slow but possible!
- You don’t need to spend a lot of money to treat plantar fasciitis initially, but more intense cases may warrant a more thorough medical approach and the purchase of items such as night splints.
What does the tissue respond best to?
Plantar fasciitis involves inflammation of the fascia, or dense fibrous connective tissue, that runs from your heel and across your arch to your big toe. Inflammation is a normal part of the body’s process in healing tissue that’s been exposed to stress. However, when the demands placed on the tissue exceed our body’s ability to repair the tissue, chronic inflammation can result.
Fascia is made up of a tissue called collagen. Collagen has the ability to repair itself, but this can only occur when repeated tensile forces are applied to it which stimulates the cells to make the tissue stronger. In the case of the plantar fascia, tensile forces are achieved when the Achilles tendon is activated and the “Windlass Affect” is achieved at the same time. The “Windlass effect” causes tightening of the plantar fascia when the toes are lifted upward (which is a common “stretching” position). The Achilles tendon can be targeted with calf strengthening (heel raises). Thus, one of the more popular exercises in the studies is a combination of both: patients perform single leg heel raises with a towel rolled up under their toes. (See “Unilateral Heel Raises” below).
The bottom line is, in order for that collagen tissue to repair itself, treatment must involve ACTIVE exercise and appropriate loading to that tissue in a gradual, progressive fashion.
What do the studies say?
A routine of stretching and shoe inserts have been shown to be effective by multiple studies, but a 2006 study by Digiovanni et al. found that 40% of athletes continued to have symptoms of pain 2 years later when their treatment was only focused on stretching.
More recent studies have evaluated the effectiveness of high intensity exercises on the tissue’s ability to heal. Similar areas of chronic inflammation in runners, such as the Achilles tendon and the Patellar tendon in the knee respond well to a training program that involves progressive high-load strength training when compared to stretching.
Researchers Ratleff et al. determined in 2014 that a heel insert and strengthening program was more effective than a heel insert and stretching program for patient outcomes after 3 months. Their exercises focused on doing single leg heel raises with a towel under their toes (see “Unilateral Heel Raises” below) and they did not incorporate any other types of exercises.
A 2015 study by Kamoneski and colleagues found that three treatment approaches were effective in treating plantar fasciitis: Foot exercises, foot and hip exercises, and stretching alone. However, those patients were only followed for two months.
Thus, it’s obvious that more research is needed in comparing a routine of stretching vs. strengthening. The exercises in this article will include a combination of both approaches, and it’s up to the individual to determine which is most effective for them. I will say that what I’ve seen in the clinic is a more optimal response when strengthening is incorporated into the treatment plan, particularly in athletes who wish to continue running for the years to come.
Getting at the root of the issue
Numerous studies have connected hip and core muscle weakness to the root cause of plantar fasciitis. When the muscles that stabilize your hips (particularly the hip lateral rotators and abductors and the deep abdominal muscles) are weak, the runner is more likely to have poor control of pronation on foot strike. This mechanism has been linked to increasing strain on the plantar fascia. Studies have also confirmed that weak calves, shin and foot muscles, and muscles that control the toes are linked to plantar fasciitis. Limited ankle range of motion in the dorsiflexion position (pumping ankle so that toes are upward) is another risk factor. Likewise, stiffness in the knees, hips or spine can also change the way you run and load at the heel. Thus, in holistically addressing the issue, muscle strength and joint mobility must be addressed to see lasting change in your running mechanics (and lasting relief!)
Those are a lot of factors to consider! This is where a consultation with a physical therapist is helpful. They can analyze your gait pattern on a treadmill and determine whether there are other factors that are influencing the stress on your plantar fascia.
On to the Exercises!
This is not intended to be diagnostic information, medical advice or exercise prescription. Always consult your physician and physical therapist prior to initiating a new exercise routine.
Strength Exercises for the Foot and Lower Leg:

Elastic band strengthening for the foot (a,b and c above)
- Attach elastic band to sturdy object as shown in picture.
- Lay on couch or table with foot off the edge.
- Pull foot outward (a), inward (b), or upward (c) against resistance of band.
- Be careful to avoid compensating with hip or trunk movement. Attempt to isolate movement to ankle.
- The study suggested performing 3 sets of 10 repetitions, once a day.
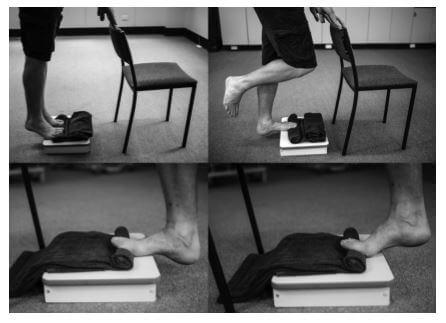
Unilateral Heel Raises (above photo)
- Find a stairway or step for the exercise.
- Place rolled towel under toes. May need to adjust several times until you feel a gentle pull on your arch with the towel underneath the toes (should not be painful).
- Perform single leg heel raises. (If you have pain, start with both legs down on step).
- Perform slowly: 3 second raise, 2 second hold up top, 3 second lower.
- One study suggests 3 sets of 12 (to fatigue) every other day, with a gradual increase in load via a backpack that is loaded with books over time. Another study suggested 3 sets of 10 daily.
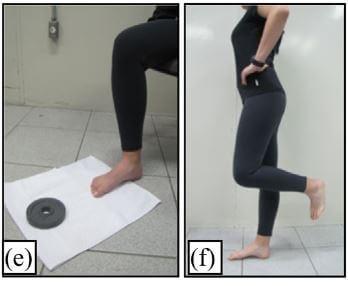
Toe Curl Exercise (e)
- Pull a towel along a smooth surface with the toes.
- Gradually add weight or small object to the towel.
- The study suggested performing 3 sets of 15 repetitions per day to strengthen the small (instrinsic) muscles of the feet.
Short Foot Exercise (f)
- Stand on one leg.
- On the standing foot, “shorten” the foot to elevate the arch, without curling your toes or removing your forefoot from the ground. Intend to bring the base of your toes toward your heel. This is a very slight/barely perceptible movement, but you should feel some tension increase in your arch.
- The study suggested performing 3 one-minute sets on each leg, once a day.
Strength Exercises for the Hips and Core
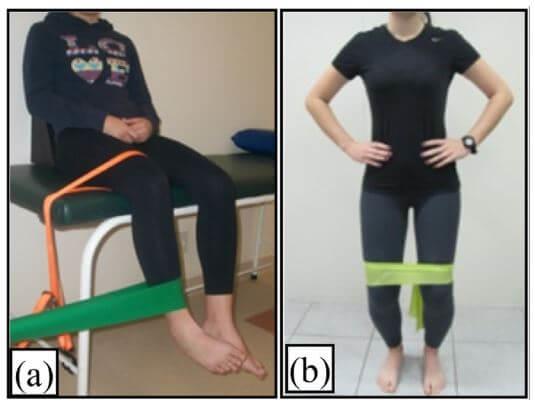
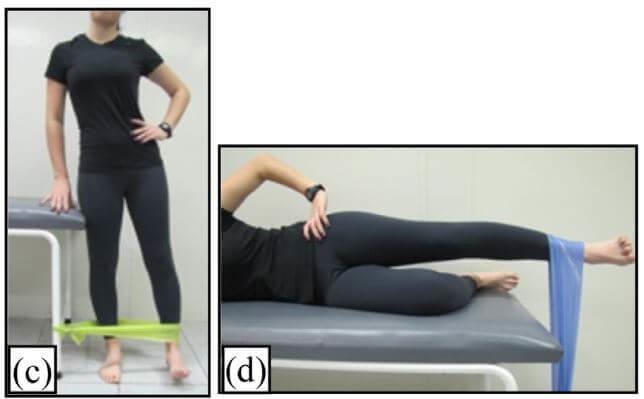
Elastic band strengthening for the hips (pictured above)
- Exercise A: rotate foot in toward other leg against resistance, without rotating thigh on the table.
- Exercise B: Side-stepping with band above knees. Keep hips level and maintain constant pressure on the band.
- Exercise C: Pull leg away from body, against resistance. Stand up straight.
- Exercise D: Laying on your side, pull leg up. Avoid rotating torso or hips.
- The study suggested 3 sets of 10 repetitions per day.

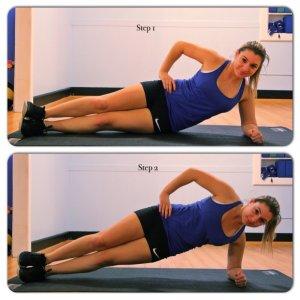
Mat exercises
- Bridging, plank, and side plank are great floor exercises to work the hip and core. Those exercises as well as the “bird dog” can be performed on the mat or advanced to something like a paddleboard for extra challenge and fun!


Single leg strengthening
- Single leg squats, bridge, side lunges and dead lifts are great exercises to combine foot loading with hip and core stability.
Stretches

Laying down Towel Stretch (a)
- Laying on your back, wrap a towel or pillowcase around your foot
- Keeping the knee straight, gentle pull the foot back toward your shin. You should feel a stretch in your hamstring and calf.
- The study suggested performing 3 repetitions of 30 second holds, once a day.

Wall calf stretch (b and c)
- Stand facing wall with a staggered stance.
- Keeping front knee bent, lean body in towards wall with arms supported on wall until a gentle stretch is felt in the calf. Keep heel of back leg on the ground.
- Alternate between the back knee being straight (b) and the back knee being bent slightly (c) to target the two different calf muscles.
- The study suggested performing 3 repetitions of 30 second holds, once a day.

Plantar Fascia stretch, seated (d)
- Cross one leg over the other.
- Put fingers on base of toes at bottom of foot and pull them back toward shin until a stretch is felt in the arch.
- Put your other hand on the arch to make sure that it feels like the plantar fascia has tension on it while you are pulling back with your other hand.
- One study suggested performing 10 repetitions with 10 second holds, 3 times per day. Another study suggested performing 3 repetitions of 30 second holds, once a day.

Active “Knee to wall” stretch (picture above)
- Keeping foot flat on floor, bend knee toward wall until you feel a pull in your Achilles tendon/calf. Pause for 1-2 seconds, return to start, repeat.
- Consider 3 sets of 30 seconds, several times per day. This will help with the elasticity of the Achilles tendon, which can impact the strain on the plantar fascia.
Dynamic Stability
These are additional exercises that we often consider in clinic before returning a patient to their full running routine. These exercises are more advanced and should always be performed pain-free. The quantity prescribed depends on many factors.


Balance training
- A progression of single leg balance in various conditions is helpful (eyes closed, standing on foam or bosu ball or grass, or with coordinated arm movements are some examples).
Box or Step Exercises
- Step-ups with eventual advancement to plyometrics can be useful loading prior to returning to competition.
Cross-training
- Numerous forms of cross-training can be performed with or without modifications as part of the recovery process. Swimming, cycling, yoga, pilates and paddleboarding are a few great examples of exercises that engage important stabilizer muscles. Get creative and have fun with it!
Additional treatment options
The American Physical Therapy Association published updated guidelines for Plantar Fasciitis in 2014. They concluded that the most supportive evidence exists for: foot orthoses (either customized or store-bought to aid with shock absorption, arch support and heel padding), taping to help reduce excess pronation with activities, manual therapy performed by a physical therapist, night splints, and stretching of the calves and the plantar fascia itself. Physical therapists have also noted success with soft tissue mobilization/massage with tools, and dry needling of surrounding or influential muscles.
Self-massage via tennis ball and ice may be used for temporary pain relief but is not widely supported as altering the injured tissue itself. Modalities such as electrical stimulation and laser treatments may be used, but are not particularly effective. Ultrasound treatment is not recommended for this injury.
Running considerations to maximize success
Rotation of shoes may be helpful for athletes and those who stand a lot at work. A rocker-bottom shoe combined with an insert is also supported in the literature for runners. Gel-based heel cups may assist in heel area tenderness and inflammation, but it’s recommended to have a full-length insert positioned into the running shoes for sporting activities.
Training considerations should also factor in the running surface. Generally, trails involve less shock than pavement and runners may do better on softer surfaces until they are symptom-free. However, aggressive (steep) or excessively uneven trails do require more dynamic hip stability and calf strength, so it’s important to slowly advance to more challenging terrain. If you are running on pavement, choose your routes wisely so that you stick to even roads and out and backs on the same side as much as possible, since angled pavement can aggravate the injury.
Lastly, don’t underestimate the importance of cross-training and rest. If you take a break from running, make it a period of “active rest” so that you are still stimulating the fascia’s collagen and preparing it for the stresses of running again in the future.
References:
Kamonseki DH et al. Effect of stretching with and without muscle strengthening exercises for the foot and hip in patients with plantar fasciitis: a randomized controlled single-blind clinical trial. Manual Therapy. 2015.
Martin et al. Heel pain – plantar fasciitis: revision 2014. J Orthop Sports Ther. 2014.
McPoil et al. Heel pain: plantar fasciitis clinical practice guidelines linked to the international classification of function, disability and health from the orthopedic section of the APTA. J Orthop Sports Phys Ther. 2008.
Rathleff et al. High load strength training improves outcomes in patients with plantar fasciitis: A randomized controlled trial with 12-month follow-up. Scand J Med Sci Sports. 2014.
Latest Articles
 Is Running on a Treadmill Easier Than Running Outside?Runners have their own preferences, whether it is treadmill running, running outside on the road, or exploring trails. So...
Is Running on a Treadmill Easier Than Running Outside?Runners have their own preferences, whether it is treadmill running, running outside on the road, or exploring trails. So... Is It OK to Use Trail Running Shoes on the Road?While trail running shoes can be used on roads, especially in situations where a runner encounters mixed terrains or pref...
Is It OK to Use Trail Running Shoes on the Road?While trail running shoes can be used on roads, especially in situations where a runner encounters mixed terrains or pref... How to Fix Sore Quads After Running?Rest, ice, gentle stretching, and over-the-counter pain relievers can help soothe sore quads after running. Also, ensure ...
How to Fix Sore Quads After Running?Rest, ice, gentle stretching, and over-the-counter pain relievers can help soothe sore quads after running. Also, ensure ... 10 Fruits With The Most Electrolytes to Replace Sports DrinksThese fruits are high in electrolytes such as potassium, magnesium, and calcium, essential for hydration, muscle function...
10 Fruits With The Most Electrolytes to Replace Sports DrinksThese fruits are high in electrolytes such as potassium, magnesium, and calcium, essential for hydration, muscle function...